Patient Spotlight: Lindsey Hofstra
It doesn’t seem to be a unique experience that those with condylar resorption, whether diagnosed or just knowing deep down there is something very wrong, must travel a long and arduous road to receive medical care. Until recently, I had undiagnosed and largely unmanaged condylar resorption that started in my teenage years.
Pre-braces images at ~10 years old.
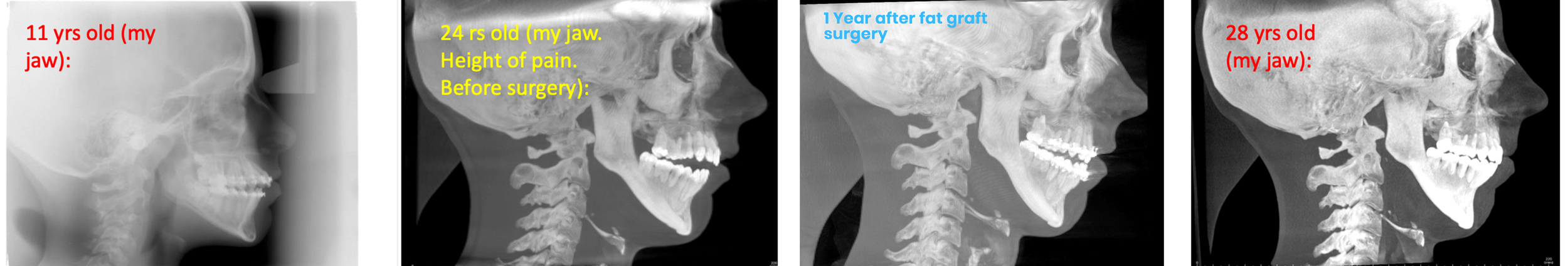
I was already somewhat retrognathic by the time I was about 10 years old and had 2 upper bicuspids removed for crowding in preparation for braces, but at least all my teeth met and I had no memorable pain or difficulty functioning at that time. I entered into braces for the first time at age 11 and what was supposed to be 2 years of normal orthodontics ended up being 4 years of extreme orthodontics, including retractive head gear and aggressive rubber band treatment.
Back then, I didn’t know that my orthodontist was battling an open bite caused by condylar resorption. After 4 years he told me that he had done “the best he could” and, even with slight gaps between my teeth, he took off my braces. Even after many years in braces, my jaw was recessed and I had an unattractive facial profile, but I had no idea that this was from braces or from my disintegrating condyles.
Image following the removal of my first round of braces (2008).
Roots of teeth over time.
As the years went on, my open bite continued getting worse and so I went back to my orthodontist. He told me that I could not ever do braces again because of how blunted the roots of my teeth were, and he failed to mention that this was caused by the aggressive treatment done during my first round of braces.
A few years later is when I started experiencing notable bouts of temporomandibular joint pain. When discussing this and my open bite with my new dentist, they told me to save up for a small house because I would need all my teeth replaced someday due to the wear and compromised roots.
Why did no one see my open bite and consider that the issues I was experiencing were related to my condyles?
After the warning from my dentist, I seemed to bounce from one misdiagnosis to another, with no doctor expressing concern for my joints, even with all the CBCT scans I had undergone.
Before undergoing any splint therapies (2012).
I continued to go to different TMJ specialists and craniofacial pain experts, and every office was quick to assert that they were the best in the business and see very complex cases. I was handed a new and expensive splint with each new doctor, with the assurance that their splint would be designed better than the previous expert. This continued for a long time and I have a large Tupperware container at home that is now full of these old splints and other orthodontia items.
My graveyard of splints.
As I carefully adhered to these different splinting plans, my open bite still grew larger and my pain only became worse. My sleep grew more restless and I felt tired and anxious constantly, most likely due to my increasingly compromised lower airway, though I didn’t realize it at the time. You can see how tired I even looked at an orthodontist’s office in the photo below.
Before any surgical interventions (2016).
As time went on, it also got more difficult for me to chew, not only from the pain I was experiencing but also from the lack of functional contact my bite had, with only 2 molars touching on either side. In 2016, when I was 24 years old, my pain had become almost unbearable, and I was still trying to perform well in a difficult graduate program with many long nights. During this time, in an attempt to try to find relief, I was driving 4 hours round trip to see another TMJ specialist and a craniofacial physical therapist. One day I began sobbing in his office, expressing to him that I couldn’t take this level of pain anymore. Thus far, my pain had been unmanaged and doctors were very hesitant to give stronger pain medicine to me because I was a younger adult. This specialist told me that my best shot at reducing my pain levels would be to have double jaw surgery to correct my open bite and bring my occlusion to equilibrium again.
With the new goal in mind, I went to another orthodontist near my grad school to start working towards getting ready for double jaw surgery. This orthodontist was the first medical/dental professional to suggest that I might have something wrong with my condyles, and that I should consult with another specialist that he knew. He said double jaw surgery would not fix my problem if I had an issue with my joints.
My dentist also recommended the same surgeon, so I immediately scheduled a consult with him, and this surgeon proceeded to tell me that my disks had slipped out and my condyles were wearing down from the disk not being in the proper position. He recommended his surgical specialty, an autologous fat graft diskectomy, explaining that the fat graft would pad the joint space and stop the resorption caused by the joint being bone-on-bone.
He also told me I might need a lower jaw surgery later if we could still not get my occlusion to meet. He felt that TMJ TJRs (total joint replacements) were a bad option, and painted a very detailed picture for me of how horrible my life would most likely be if I went that route. I was in so much pain and so desperate to get out of it that I agreed to have the surgery, which insurance approved (but later discounted the costs so heavily that I was only reimbursed about 3% back of my total surgeon’s fees). It was a long and hard recovery during my last semester of grad school.
Splint and banding following my fat graft surgery.
Navigating life with my splint and bands.
I spent about 6 months being banded in my surgical splint and was heavily medicated to the point that I didn’t really feel like myself anymore. I even gave project presentations with my mouth banded shut… I was very committed to following every protocol my surgeon gave me. I then spent a little over 2 years in braces to intrude my back molars for the second time, and extrude my front teeth. I graduated from grad school and entered into my first job with braces and still on a soft chew/liquid diet to support the healing of my fat graft surgery.
The diskectomy got my bite to meet up a little better, but both the fat grafts and my condyles started to resorb more during this time. The surgeon later told me that it was normal to have a little more resorption during this healing process – I wish that had been told to me before I did the surgery.
Braces came off and my pain had improved, though it still required several medications to manage (even 2 years later), but within 2 months of the braces being off my bite started to open back up again.
I was devastated and I was still in pain.
Detailed timeline of my experience with pain and condylar resorption.
(click here for larger view)
I still trusted this office and was told that we could do an upper jaw surgery to correct my open bite, which they later changed to be only SFOT (surgically facilitated orthodontic therapy), where we would further intrude and extrude my teeth for the 3rd time. Everyone thought this was the best treatment plan for me, but I hit a mental breaking point and thought, “I will always be spending time, mental energy, and money to close this open bite, won’t I?”
Progression of anterior open bite over time.
This is when I began looking for other people online who might have my “strange” jaw joint condition, too. I began to join jaw surgery groups on Facebook and post my scans and story, thinking I might find maybe 5 other people in my state that had my issues. I knew so little back then. I was told to join the Idiopathic Condylar Resorption group, even though I didn’t really know what that was, and shared my story there. I was shocked, but also validated, in finding out that I was in really bad shape. I finally had other people’s scans and stories to compare with mine, and felt that I finally had access to all the right information I needed to control and make decisions on what would be best for my health.
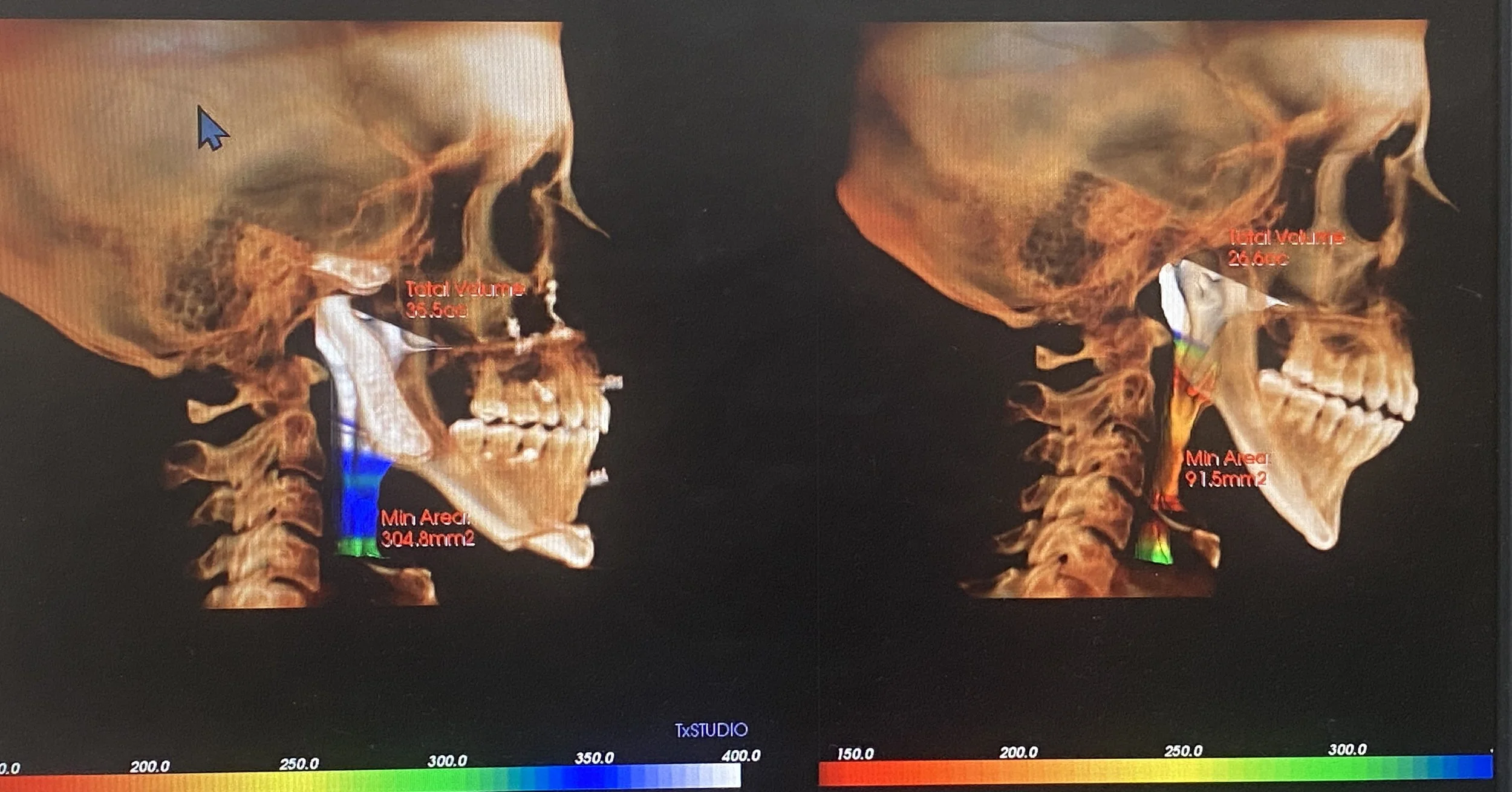
Thinking about my health and trying to figure out all the puzzle pieces became like a part time job. There was a lot to figure out… what doctors could I trust? I had given my trust to so many doctors in the past who were so sure of their treatment plans, only to have my health progressively worsen. I began to mentally register sleeping issues that I had from other group members sharing their symptoms and was officially diagnosed with UARS (upper airway resistance syndrome), with the narrowest portion of my throat spanning just 2.01mm.
The size of my airway.
Who knows how long I had had UARS for or the issues that have been caused from not being able to sleep properly for years and years. I also wondered how many of my other issues were related to my jaw and my orthodontically manipulated skeletal structure.
Cephalometric scans over time.
At this point in my journey, 13 years had passed from when I had first returned to my childhood orthodontist to address my increasing open bite.
Meal time on a blended diet.
I proceeded to get 4 additional opinions on top of my first jaw surgeon’s, and they all recommended the exact same treatment to me. Bilateral total joint replacement, LeFort, and genioplasty. My symptoms grew worse as I began to choke awake more and more from my airway closing, and I began to worry about choking when I ate, even though I was blending or liquifying almost all of my food by this point.
Eating was a very emotional process and many times I would just avoid eating to not have to deal with the pain or difficulty of it. In preparation for my next surgery, I continued researching and talking with other patients online. I proceeded with SFOT+MSE surgery in May of 2021 in an effort to provide more bone around my teeth since I was at risk of losing them with the additional orthodontic treatment required for my TJR surgery in 2022.
Left: Airway after TJR. Right: Airway before TJR.
I have now had my TJR surgery and I am still in orthodontic treatment as I write this, but I am doing much better than I once was with far less pain and sleeping better with my improved lower airway. I did have a complication from my surgery involving my septum deviating almost immediately afterwards, so I have been meeting with different ENT+Plastics doctors since about a month after my jaw surgery and have been given different treatment plans. It seems to be a somewhat complex deviation that will most likely need a rib graft to fix and I have learned just how complex the nose is and how common nose surgery revisions are even for regular rhinoplasties. Even with the improvements, it truly feels like my medical needs continue to revolve around my jaw, so there have also been some hard days after surgery. Right now, fixing the deviated septum is high on my priority list because it makes it difficult for me to breathe through my nose at night and sometimes during the day. It is also disheartening to look in the mirror and see my new face with a crooked nose, but I hope that these feelings become better with time and with having my nose fixed.
Despite these ongoing tribulations, I do feel that I found the right treatment and wish that I had had access to information on condylar resorption sooner. I wish we understood the reasons that condylar resorption even occurs so that we could prevent others from having to go through this. I feel like I have lost so much of my life and personality to having to manage this – chronic pain, disordered sleep, losing my ability to function and chew, money spent on specialists, time wasted, mental and physical energy spent, and anger from being misdiagnosed for so long from the lack of education on this condition in the medical community. Dental and orthodontic work are not quick solutions and these drawn-out treatments, can sometimes span half a decade or more, all without the promise of relief. The ever-present risk of aggravating condylar resorption symptoms further with these treatments is a real worry, but medical professionals unfamiliar with condylar resorption may just ascribe any pain or complications to being a needy patient. In my case, to add insult to injury, these treatments weren’t even what I ultimately needed to fix my condyles and stabilize my bite.
I am happy that I (eventually) found a treatment option that was best for me, but I struggle to accept that there are other people like me out there, right now, undergoing braces, orthotic treatments, double jaw surgeries, diskectomies, dental adjustments, and any other treatments that may not be appropriate in treating undiagnosed condylar resorption patients. Having TMJ issues are, for whatever reason that I cannot fathom, massively overlooked in the medical field. Even medical and dental insurance often argue over who is ultimately financially responsible for helping patients needing TMJ-related treatments. My hope is that others who are dealing with condylar resorption will have brighter futures through educating both doctors and patients on this condition. I hope that in sharing my story I have provided a glimpse into what I and so many others have had to go through to do something as simple as chew and breathe.